7 creative self-care techniques for neurodivergents
Do you struggle with self-care as a neurodivergent (ND)? You may not be the only one.
Surviving in ableist societies can be taxing for many ND folks at the best of times. We may spend all our energy just trying to fit in—energy we may otherwise need for rest and recharging.
Added to this, many self-care techniques can feel like a chore, especially when we are pressed for time.
Trying to squeeze one more thing into an already overburdened schedule when we’re already feeling overloaded can be particularly anxiety-provoking.
I remember once upon a time, the very idea of pausing to do meditation or a yoga class was enough to send me into a tailspin.
“That’s 20-30 minutes I’ll be losing from my schedule,” I would think. “20-30 minutes I don’t have!”
Given much of my workload was self-generated as a result of ADHD workaholism, my sense of urgency around time in retrospect didn’t make a whole lot of sense.
No one after all was demanding I submit a script in time for three different competitions. The deadline I had set for finishing my feature documentary was of my own devising.
The pressure of being a multi-passionate autistic
The issue in my case had to do with my fixating on the gap between where I was and where I wanted to be. I was a multi-passionate autistic and ADHDer with an array of interests I knew I could excel at…if only I knocked on the right doors and made the wrong connections.
This unsurprisingly is where I struggled most. NDs face very real obstacles with social communication and interpersonal relationships. And yet I told myself that I could ignore these obstacles. Sooner or later, my labors would yield fruit.
And so I continued to work in isolation, in the service of various passions that I hope to turn into viable careers.
After years of this, I began to feel rather hopeless about it. What, after all, did I have to show for all my effort, save a few life experiences and college degrees?
My dissatisfaction drove me only further in my pursuit of achievement, which in turn made my self-worth dependent upon that pursuit.
The time pressure I thus experienced was not the result of external circumstances but toxic self-perceptions. I didn’t believe myself to be “good enough” or deserving of self-care until I had first “made it”. Yet failing to care for my own needs only increased my anxiety and this sense of time pressure.
For other NDs, external circumstances may indeed pose a very real obstacle to self-care. When we are strung out between the pressures of operating in a neurotypical (NT) world, alongside commitments such as work, school, family, and social lives, self-care activities certainly start to seem onerous, if not out of the question.
Yet no matter how strong the impulse might be to put downtime on the back burner, without adequate rest and rejuvenation, our ability to fulfill these commitments and pursue our passions will suffer.
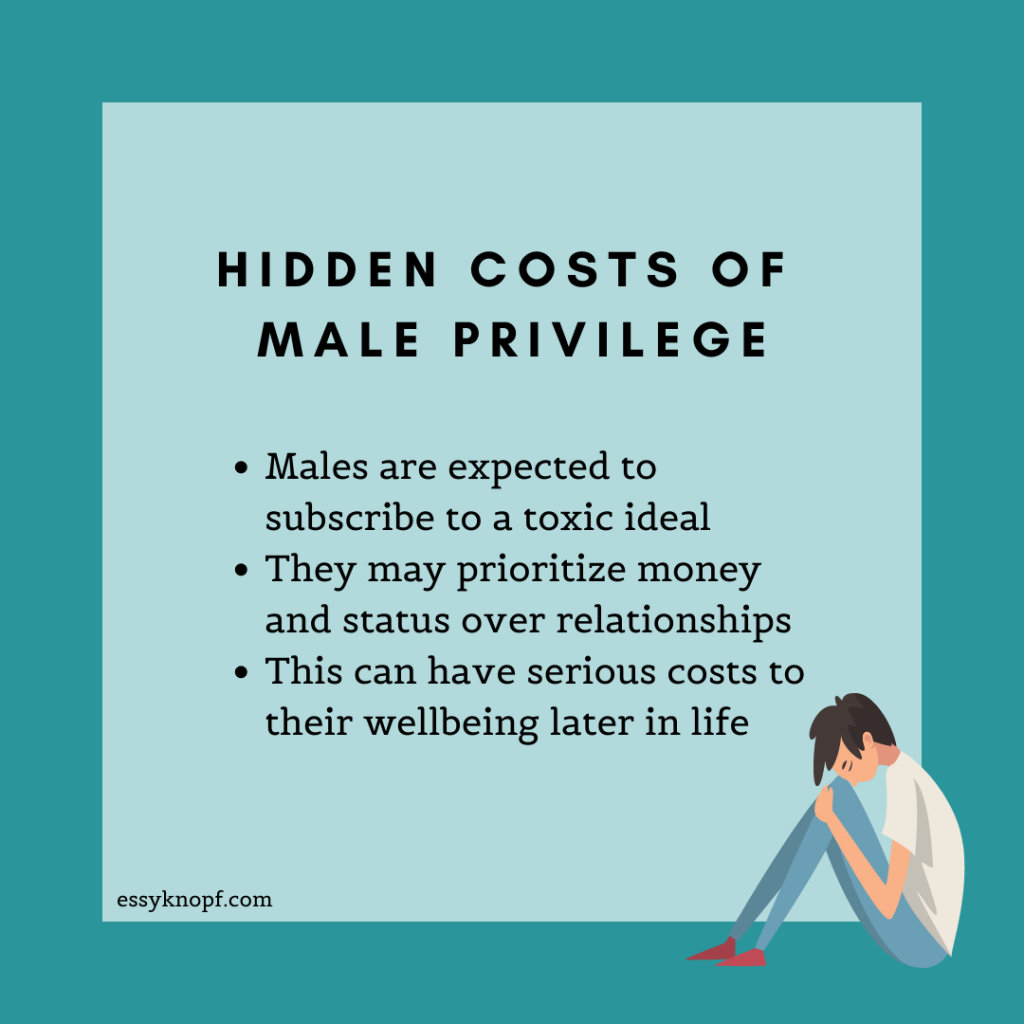
Should self-care techniques such as getting a massage or drinking water fail to appeal to you, consider exploring the following seven simple and unorthodox methods.

1. Shower mindfully – an unexpected NT self-care activity
Don’t have time to recline in a bath? Not a fan of bubbles and scented soap? That’s okay.
If being pummeled by hot water is more your jam, follow this quick 5-minute guide to increasing your shower pressure.
Next, shake up your mindfulness routine by trying this exercise while standing under your showerhead.
2. Shop guilt-free
Retail therapy can indeed have therapeutic benefits, but in excess, it can create debt that negatively impacts our mental health. Know however that self-indulgence doesn’t have to hurt your pocketbook.
Visit a discount store with low-priced items. Hunt down little items you might not otherwise have budgeted for, but which you know will add some value or comfort to your life.
For example, a shower caddy, plastic storage tubs, or a new drink bottle.
Whatever you end up buying, know that it is the act of spending money that generates the “feel good” feelings typically associated with retail therapy.
This way you’ll get all the benefits with none of the financial strain—or buyer’s remorse.
3. Have a lie-in
Pick a morning when there are no pressing matters to attend to and simply stay in bed.
Alternatively, use your morning to complete errands and spend the remainder of your day under the covers.
Make whatever adjustments are necessary to maximize comfort. Turn on your air conditioner, close the blinds, put your phone into airplane mode, make a cup of tea, light a scented candle, or switch on an essential oil diffuser.
If relaxing still proves difficult, and you find yourself battling anxiety, consider donning a weighted blanket or a compression vest.
These use deep pressure to help ease anxiety and are available to purchase online.
4. Ritualize a mini-hobby
Many hobbies require time and energy we aren’t always able to spare. If this is your experience, consider expanding your definition of the word “hobby”.
For instance, I was never much one for comedy, save for watching the odd opening monologue from a late-night talk show, schedule allowing.
When I discovered that these shows made a perfect accompaniment to my breakfast routine, I understood that maybe time wasn’t an issue after all.
Sure, enjoying Jimmy Kimmel, Samantha Bee, John Oliver, Seth Meyer, and Stephen Colbert isn’t strictly a hobby. Yet it can impart many of the usual benefits, such as supporting mental health and relaxation—in this case, through laughter.
By incorporating a mini-hobby like this into your day, we will stand a better chance of making it a habit, ensuring it survives peak periods of busyness.
In order to create a habit, we not only have to do it regularly—we also have to follow the four laws of behavioral change, as described by Atomic Habits author James Clear:
#1 Make it obvious.
#2 Make it attractive.
#3 Make it easy.
#4 Make it satisfying.
In my case, the enjoyment provided by watching these videos fulfilled law #4 (“make it satisfying”).
In order to “make it obvious”, I subscribed to each comedian’s dedicated YouTube channels so that their most recent videos appeared on my homepage.
By keeping my YouTube homepage always open in a browser tab, I enhanced the attractiveness of these videos (“make it attractive”).
And by waking up early, I was able to eat and perform my new ritual at my own pace (“make it easy”).
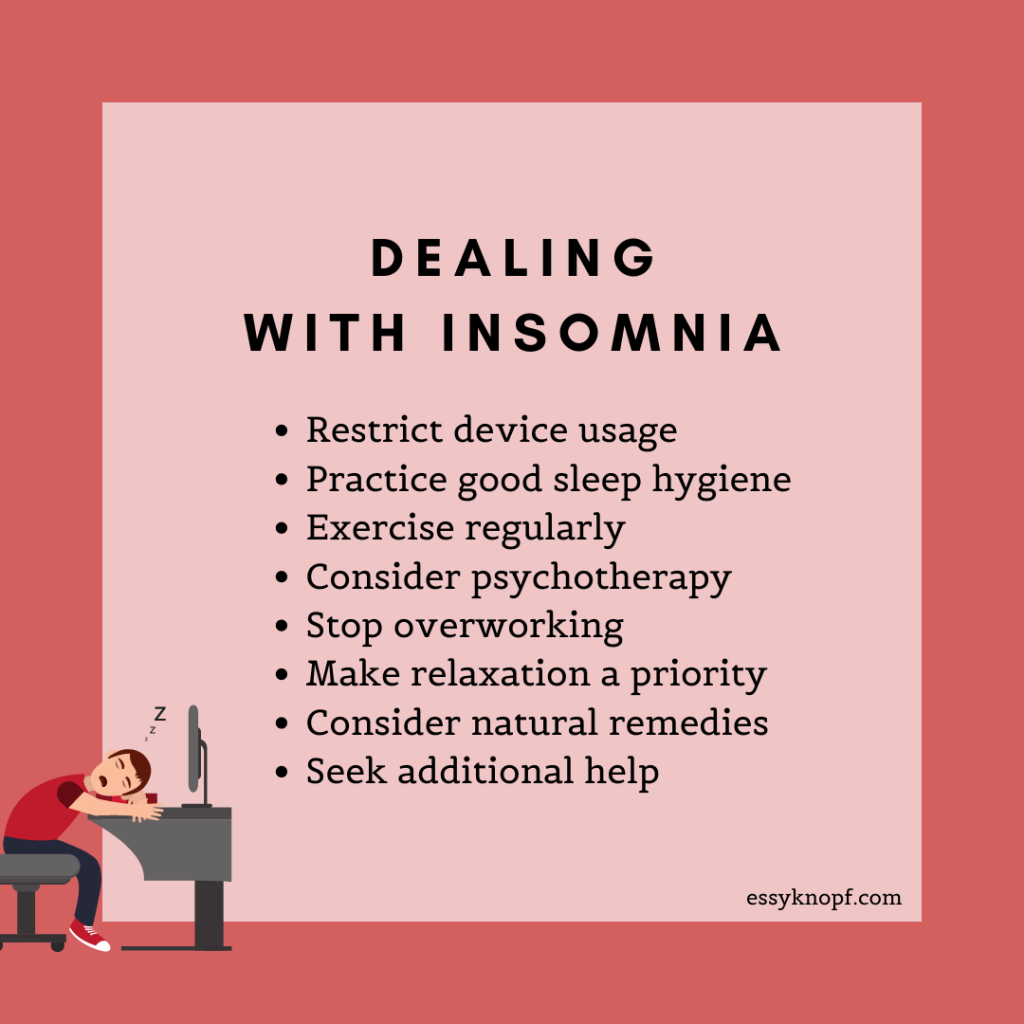
5. Take a power nap
Napping isn’t just the favored activity of layabouts—it’s also a super effective way to give your flagging energy levels a boost!
If your workplace doesn’t look favorably about employees taking catnaps, a quick lie down after a taxing day can help restore you.
Naps of between 10-20 minutes are considered ideal, as anything longer than 30 minutes can leave us feeling groggy upon waking.
Napping not only decreases sleepiness but can improve learning and memory while supporting the regulation of our emotions.
6. Get some green therapy
The emerging discipline of green therapy—also known as ecopsychology—is concerned with using nature to help us recharge our internal batteries. Multiple studies have demonstrated that the presence of nature can have a plethora of health benefits.
Venturing into the wilds may not always be possible, but you can reap the same benefits from visiting your local park. Twenty minutes as it turns out can be enough to relieve stress.
You reap similar effects using simulated green spaces. For instance, by placing fake plants around your home or workspace.
Another method involves slipping on a pair of headphones and listening to natural sounds, such as wind through trees or running water.
7. Try audio bibliotherapy
The act of sitting down to read a book in today’s helter-skelter world is becoming increasingly uncommon. But if you lack the patience to read the conventional way, you can always try listening to an audiobook instead.
Having your books read aloud to you can be an effective way to consume content without having to add to your already overburdened schedule.
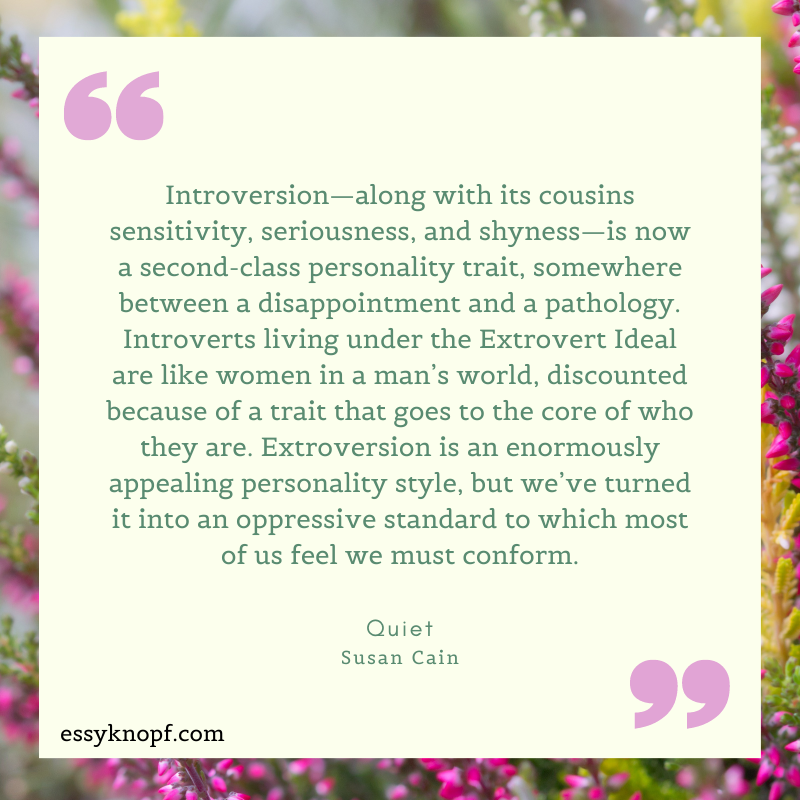
Furthermore, if you’re suffering work-related stress or battling anxiety and depression linked to your busy lifestyle, reading books about these challenges can go some way to lighten your load and help you apply self-care techniques.
Healing through reading is known as “bibliotherapy”, and it can serve as a wonderful resource for those among us struggling to access support networks or the sympathetic ear of a therapist.
Books that teach self-care techniques
There is no one-size-fits-all solution to the challenges mentioned above. But if you aren’t able to invest the time to seek out personally appropriate guidance, consider exploring the following recommendations:
- For dealing with stress: Full Catastrophe Living – John Kabat-Zinn
- For depression: Feeling Good – David D. Burns
- For anxiety: When Panic Attacks – David D. Burns, The Places That Scare You – Pema Chödrön
- For dealing with difficulties: When Things Fall Apart – Pema Chödrön
- For making peace with your mind: The Happiness Trap – Russ Harris
- For setting boundaries (including at work): Boundaries – Henry Cloud & John Townsend
- For learning how to practice self-compassion: Self-Compassion – Kristin Neff
8. Start a self-compassion practice to round off your self-care
Build a deliberate self-compassion practice with the support of the many free, downloadable resources on the Self-Compassion website.
Author Kristin Neff has prepared brief guided practices, a list of exercises, and tips for those new to the concept.
Finally, if you have a habit of going too hard on yourself and zeroing in on your supposed deficits as an ND, try adopting a strengths-based perspective.
Instead of looking at yourself as somehow flawed, acknowledge the many strengths that come with being ND, which I explore in another blog post.

Essy Knopf is a therapist who likes to explore what it means to be neurodivergent and queer. Subscribe to get all new posts sent directly to your inbox.