Can’t sleep? Here are some surefire steps to treat insomnia
As a teenager, I was anxious, isolated, and afflicted with insomnia.
Most days I spent indoors, indulging in geek interest escapism. Sometimes I would craft elaborate fantasy and science fiction stories. Other times I would voraciously consume books, movies, and video games.
Refuge could also be found, of all places, in hammering out essays at the computer. (That such projects could bring order to my otherwise unpredictable school and home life probably speaks to the systematizing nature of my autistic brain.)
The downside of my constant computer use was that relaxing became difficult. A day spent glued to my screen would inevitably leave my mind restless, my sleep broken.
Still, I continued to return to my computer, until what had begun as escapism gradually turned into workaholism.
Table of contents
Developing insomnia
Without friends, family, and a community to ground me, my self-worth became proportional to my productivity. There was always more to do, one more task needing completion.
Trapped in a vicious circle of feeling isolated, I sought reprieve in workaholism, which in turn only exacerbated my loneliness.
Living with constant internal pressure was motivating and could even be affirming. Just look at how productive I was being! So what if my peers at school bullied me – just look at these shiny achievements, these notches in my academic belt!
Caught on a treadmill of what I would later recognize as grandiosity, and terrified of the fall that would follow the moment I stepped off it, I became mired in anxiety and depression.
But rather than slowing down, I ramped up my commitments. At the height of my workaholism, I found myself juggling a full-time job, a feature documentary, a web series, a novel, and organizing two research trips abroad.
Getting to, and staying, asleep by this point had become an elaborate, multi-staged ritual, beginning with a double dose of Benadryl, followed by an hourlong walk around the neighborhood while I waited for it to take effect.
Sometimes I would end up at a 24-hour gym, working the elliptical until the fatigue hit me…unaware that all this activity was probably only making my objective all the more difficult.
When I got home, I’d pull my blackout curtains, slip on an eye mask, put in my earplugs, fit a pair of headphones, cue a soothing audio track, and lie down on a makeshift bed on the floor.
This, of all places, was the only place I was guaranteed to nod off, for reasons I still don’t understand. After many a tossing, turning and blanket adjustment, I’d doze off, only to wake a short while later.
Climbing into my real bed, I’d return to sleep, to rise the following morning, still tired but wired, ready to chip away at my ever-growing workload.
Some nights, however, I would doze off, only to be woken by a hypnic jerk, a kind of whole-body twitch typically preceded by the sensation of falling.
Again and again, I would doze off, only to be jerked wide awake. The steady background hum of anxiety would be cranked up into a shrill roar, putting sleep still further out of reach.
The journey towards recovery
Self-generated projects until this point had been the main source of meaning in my life, and yet they were as much a palliative as they were problematic.
The comparative ease with which others were able to accomplish sleeping – a basic bodily function – told me that something in my case had gone awry. Believing there was no recourse, however, I kept up my unwieldy sleep routine for years.
My mother’s staunch opposition to any form of dependency made prescription medication seem like a false option. Sure, I was already relying on Benadryl, but then again antihistamines weren’t habit-forming drugs.
And even supposing I could scrape together enough money to get a proper diagnosis, I would have to contend first with the fear that the professional I saw might dismiss my problem outright.
The situation reached a tipping point one night while I was doing my regular insomnia shuffle around the neighborhood, I became caught in a rainstorm.
Any sensible person would have run home, or at the very least ducked under the cover of a tree. But to return home before the Benadryl took effect would mean yet another sleepless night. So I pushed on.
The wind picked up, turning the rain horizontal. Next thing, it was inverting my umbrella, leaving me exposed to the elements.
After about half an hour of this, I surrendered and trudged home, sloughing off my dripping clothes and climbing into bed.
When sleep did not come, I grew increasingly anxious. The anxiety snowballed into hypnic jerks, which in turn fueled the anxiety.
The night stretched on, each hour punctuated by an anxious glance at my phone screen to check the time. Heavy with the dread of facing a new day unrested, I lay there, waiting for my morning alarm.
Come the following night, I still couldn’t sleep, and my insomnia ballooned into a record 50-hour spell that only ended with a no-refill script for Valium.
The doctor I saw granted me this small mercy on the condition I see a sleep specialist. The specialist in turn requested I visit a sleep clinic.
Two weeks later, I packed my bags like someone preparing for a red-eye flight and drove through the dead of the night to the evening ghost town of a local business district.
Strolling through a deserted highrise lobby I was overtaken by the peculiar feeling I was participating in some secretive, perhaps even illicit activity.
The elevator opened to the clinic’s front desk, where I was greeted by a man in scrubs who directed me to a sleeping cubicle.
After having changed into my pajamas, I stretched out on the bed as countless electrodes were attached to my head and chest until I resembled some primitive robot trailing electrical cables and hydraulic tubes.
Just how exactly did these people expect me to get to sleep?
The thought of it alone caused my anxiety to surface. Palming a pill, I settled into bed and waited for the heavy embrace of drug-induced sleep.
Seven hours later, I woke to the nurse removing electrodes. Hollow-eyed, I dressed then shuffled like a zombie from the room.
Treating insomnia
“So far as I can see,” the sleep specialist said, poring over my results, “you have a perfectly normal sleep cycle.”
I frowned my disagreement.
“So why am I struggling to fall asleep?” I pressed.
Alas, the specialist had no answer for me. Instead, he suggested an alternate treatment for my anxiety, something known as biofeedback.
A round of treatment would cost something in the range of five thousand dollars – an expense my insurance company was unwilling to subsidize.
With my wallet still smarting from the cost of other, unrelated illnesses, I turned to my final recourse: pharmacological treatment.
Explaining my long-standing problem to my psychiatrist, I caught myself making excuses.
“I don’t want to rely on drugs,” I said, “but this problem has gotten way out of control.”
“Well, it sounds like you’ve tried everything else,” my psychiatrist replied. “Don’t you think you deserve some relief?”
“Maybe,” I thought, feeling nevertheless that I had, in some unexplainable way, compromised my integrity.
With there being no one-size-fits-all medication for anxiety, I would now have to navigate a gauntlet of medications.
The most popular option was selective serotonin reuptake inhibitors (SSRIs). Think Lexapro, Prozac, and Zoloft.
Mainstream SSRIs however come with certain unpleasant side effects. After a couple of doses, my libido took a total nosedive.
The next recommendation was an antipsychotic medication that left me foggy-brained. One morning, while still under its spell, I pulled out into traffic, miscalculated my timing, and was almost hit by another car.
Fearing I might not be so lucky next time, I switched to a combination of antidepressants and antianxiety drugs. Thirty minutes after taking my first dose, I fell into a deep sleep.
When I woke eight hours later, it was to the discovery that the insomnia problem I had been battling for more than 15 years was, more or less, gone.
No more frazzled nerves, poor concentration, and feeling dead on my feet. As for the constant companion that was my anxiety? His hands had now been prized from the steering well and his butt relegated to the backseat.
Before, sitting down for 15 minutes to meditate had been an exercise in self-torture, my thoughts flinging themselves in every which way in a bid to escape any semblance of control.
With the current chemical cocktail, however, I was suddenly able to achieve some degree of focus.
Insomnia is a modern epidemic
Sure, these pulls could put a cap on my anxiety and insomnia – but they couldn’t completely suppress it.
In moments of stress and overcommitment, my mood disorder would flare up again, offering proof that if I wanted to truly get better, I would need to take a more holistic tack.
This in short would involve psychotherapy, undertaking a regular meditation practice, and making daily relaxation time a priority.
It also meant addressing ongoing insomnia triggers, such as an overreliance on digital devices, and workaholism as a coping mechanism for social isolation.
My challenges as I quickly realized were not exclusive to me. Smartphone dependency and “the cult of busy” as we all know are almost universal features of modern life in the West.
Some critics have even called our times an “age of distraction”, with obsessive work and device exposure creating conditions ripe for mental illness.
Even when faced with the physical and psychological manifestations of our stress, we often try to ignore them – much to our detriment.
Finding a solution that works for you
If there’s anything my journey to overcome insomnia has taught me, it’s that we can’t ignore our problems or rely on Band-Aid fixes.
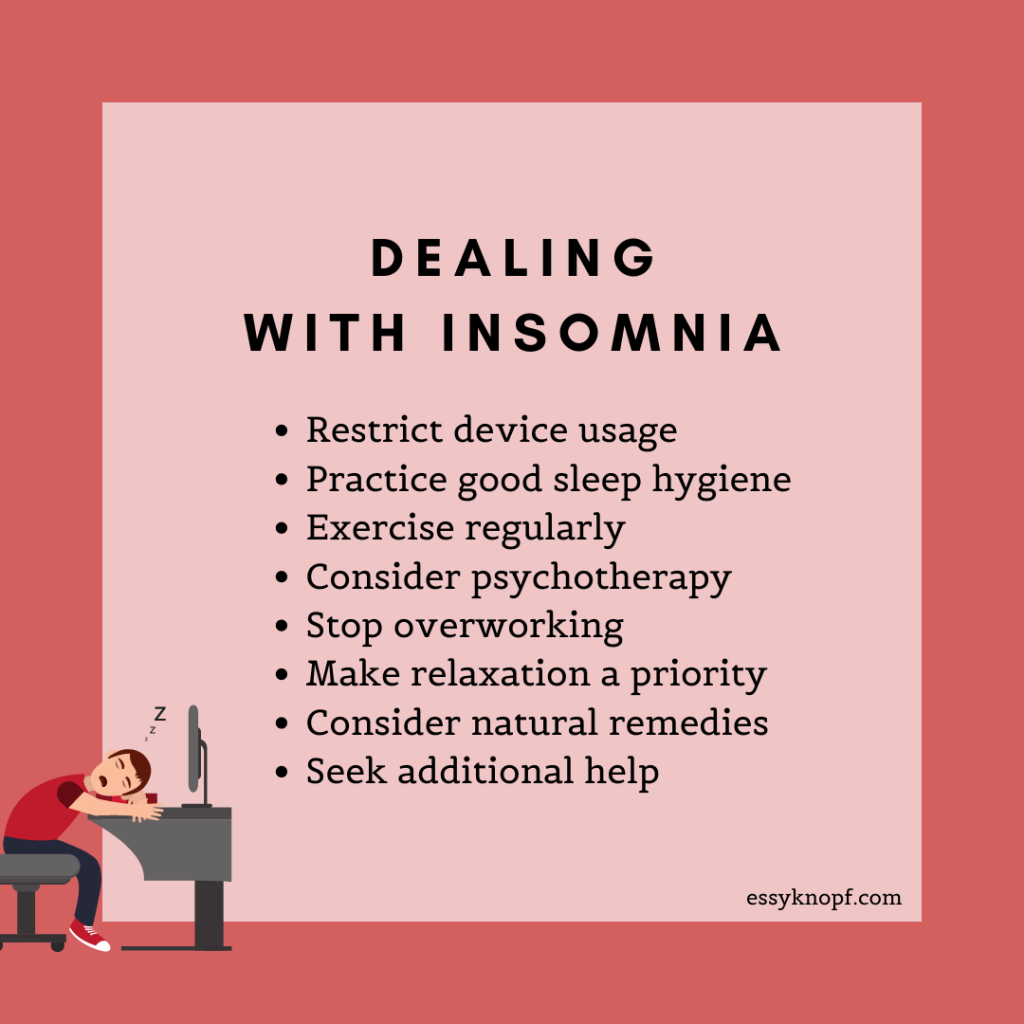
Those of us who are looking to kick our sleep woes to the curb can find some relief by adopting one or more of the following changes:
Restricting device usage: Use the wellness feature on your Apple or Android devices (sometimes referred to as “night light”). This reduces the amount of blue light emitted around set times. This light can have the effect of keeping your brain in “awake” mode. It’s also worth turning on your phone’s do-not-disturb mode and enforcing a no-device usage rule around bedtime.
Practice good sleep hygiene: Create ideal conditions for sleeping. Go to bed and get up at a regular time. Ensure your bedroom is quiet, dark, relaxing, and comfortable. As an addendum to the first point, try to remove electronic devices from your sleeping space. Employ blue-light-free bulbs. Avoid large meals, caffeine, and alcohol before rest. Use your bedroom exclusively for sleeping. More tips here.
Exercise regularly: Keep physically active during the day. Dispel depression, anxiety, and restlessness with a daily gym routine or aerobics workout.
Consider psychotherapy: Therapy can provide a safe outlet for pent-up emotional tension, which can in turn affect your ability to sleep. Therapy can also support your efforts to develop coping strategies.
Stop overworking yourself: Identify an eight-hour daily working window. Use hacks to enhance your productivity. Exercise self-discipline to stop work spilling over into “you” time.
Make relaxation a priority: You can’t be productive if you’re feeling depleted. Replenish your inner reserves every day with fun and enriching activities. Catch up on your favorite TV show, take your dog to the park, or try a new recipe. Consider doing meditation, breathing exercises, or yoga to help you unwind. Adopt what Jon Kabat-Zinn calls a “non-striving” attitude.
Consider natural remedies: While Benadryl can assist with occasional insomnia, natural treatments like melatonin, valerian root, magnesium supplements, lavender, and passionflower extract may prove equally effective.
Explore additional help: Attend a sleep clinic. Explore alternate therapy options. Seek the guidance of a psychiatrist. Investigate prescription medication.

Essy Knopf is a therapist who likes to explore what it means to be neurodivergent and queer. Subscribe to get all new posts sent directly to your inbox.
© 2025 Ehsan "Essy" Knopf. Any views or opinions represented in this blog are personal and belong solely to the blog owner and do not represent those of people, institutions or organizations that the owner may or may not be associated with in professional or personal capacity, unless explicitly stated. All content found on the EssyKnopf.com website and affiliated social media accounts were created for informational purposes only and should not be treated as a substitute for the advice of qualified medical or mental health professionals. Always follow the advice of your designated provider.